Venetoclax-based regimens for NPM1-mutated AML
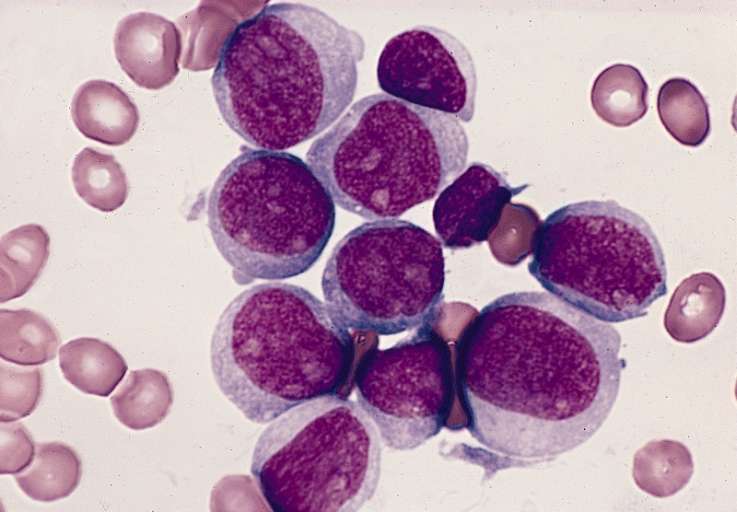
The molecular chaperone nucleophosmin-1 (NPM1) is involved with cellular epigenetic regulation through nuclear-cytoplasmic protein shuttling, ribosomal assembly, and the maintenance of cellular senescence via interactions with the tumor suppressor p53.1-2 NPM1 is frequently translocated or mutated in hematological malignancies.3 Indeed, in acute myeloid leukemia (AML) patients exhibiting distinctive biological and clinical features, mutations of NPM1 leading to aberrant cytoplasmic dislocation of nucleophosmin (NPMc+) appear in about one-third.4
Despite NPM1+ typically being associated with a more positive prognosis, this benefit becomes reduced with increasing age in patients treated with standard intensive chemotherapy (IC) or hypomethylating agents (HMAs).
A retrospective analysis published in Blood Advances investigated the outcomes of patients with NPMc+ AML treated with one of three induction therapies: HMA plus the BCL-2 inhibitor venetoclax (VEN), HMA alone, or IC therapy alone.
The following key results were found:
• In patients treated with HMA plus VEN, HMA, or IC, a composite complete response (CRc: CR + CR with incomplete count recovery) was seen in 96% (27/28), 36% (17/47), and 89% (204/228) of patients, respectively (HMA plus VEN vs HMA, P < .001; HMA plus VEN vs IC, P = .10).
• The CR rates in patients >65 years old treated with HMA plus VEN, HMA or IC were (23/26) 88%, (11/39) 28%, and (14/25) 56%, respectively (HMA plus VEN vs HMA, P <0.001; HMA plus VEN vs IC, =0.01).
• Patients aged >65 years treated with HMA plus VEN had a significant improvement in overall survival (OS) compared with HMA or IC alone (not reached [NR] vs 0.4 years; P < .001 and NR vs 0.93 years; P = .001, respectively).
• OS was 80% after median 1-year follow-up in older patients treated with HMA plus VEN, with an estimated 2-year OS of 70%.
• Multivariable Cox model analysis revealed HMA plus VEN to be associated with a 69% lower risk of death compared to IC (hazard ratio, 0.31; 95% confidence interval, 0.12-0.83; type I error–adjusted P = .038).
In conclusion, HMA plus VEN combinations displayed impressive results compared with traditional standard-of-care regimens in older patients with NPM1+ AML, and therefore, could be considered as a mutation-targeted treatment option for this population.5
Written by Thomas Southgate
References
- Colombo E, Marine JC, Danovi D. Nucleophosmin regulates the stability and transcriptional activity of p53. Nat Cell Biol. 2002;4(7):529-533.
- Falini B, Mecucci C, Tiacci E, et al. GIMEMA Acute Leukemia Working Party. Cytoplasmic nucleophosmin in acute myelogenous leukemia with a normal karyotype. N Engl J Med. 2005;352(3):254-266.
- Falini B, Nicoletti I, Bolli N, et al. Translocations and mutations involving the nucleophosmin (NPM1) gene in lymphomas and leukemias. Haematologica. 2007;92:519–532.
- Falini, B, Bolli N, Liso A, et al. Altered nucleophosmin transport in acute myeloid leukaemia with mutated NPM1: molecular basis and clinical implications. Leukemia. 2009;23:1731-1743.
- Lachowiez CA, Loghavi S, Kadia TM, et al. Outcomes of older patients with NPM1-mutated AML: current treatments and the promise of venetoclax-based regimens. Blood Adv. 2020 April;4(7):1311-1320.