Brexucabtagene autoleucel receives FDA approval for R/R B-ALL
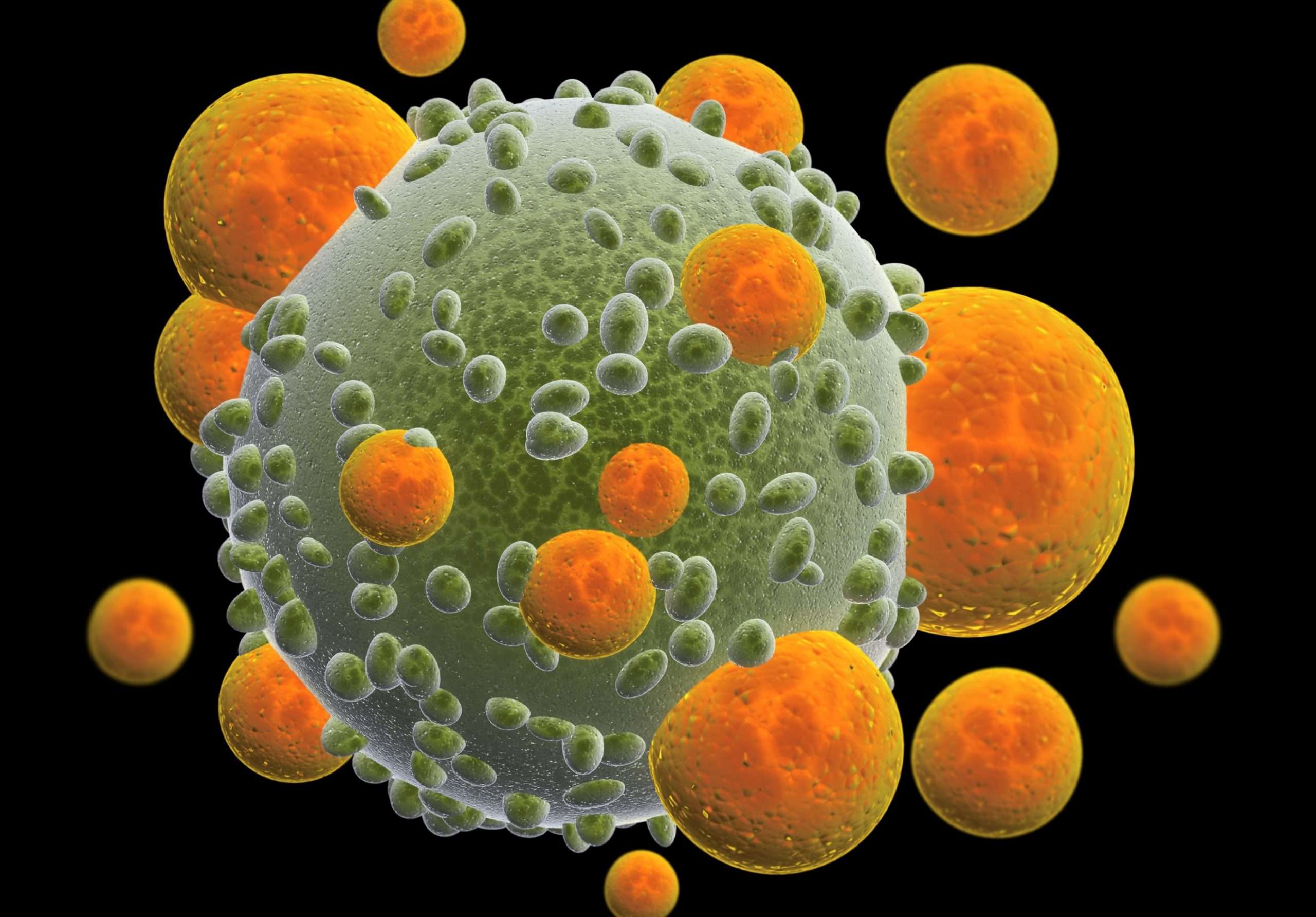
On October 1, 2021, the US Food and Drug Administration (FDA) approved the use of brexucabtagene autoleucel, an autologous CD19-directed chimeric antigen receptor T-cell (CAR-T) therapy, for the treatment of adult patients with relapsed or refractory (R/R) B-cell precursor acute lymphoblastic leukemia (B-ALL). The approval of brexucabtagene autoleucel was based on results of the Phase I/II ZUMA-3 trial (NCT02614066).1
Although high response rates to frontline therapy are observed amongst adult patients with B-ALL, 40-50% of patients relapse, resulting in a poor prognosis, with a one-year survival rate post-salvage therapy of 26%.2 Whilst the novel agents blinatumomab and inotuzumab ozogamicin have helped a proportion of patients achieve complete remissions, overall survival rates remain below eight months and are dependent on consolidation with allogeneic stem cell transplant, an option which is not available to all patients, thus presenting an unmet medical need.2
The ZUMA-3 trial is a single-arm, open-label trial, evaluating the safety and efficacy of brexucabtagene autoleucel in patients with R/R B-ALL. In the trial, patients received a single infusion of brexucabtagene autoleucel following completion of lymphodepleting therapy. At a median follow-up of 16.4 months, 39 patients had achieved a complete remission or complete remission with incomplete hematologic recovery (71%; 95% CI 57-82), with 31 (56%) achieving a complete remission. The study reported a median duration of remission of 12.8 months (95% CI 8.7-not estimable). For patients who responded to brexucabtagene autoleucel, 97% achieved measurable residual disease (MRD) negativity and the median overall survival was not reached.2
The study also found that brexucabtagene autoleucel had a manageable safety profile. The most common treatment-related adverse event (TRAE) of grade 3 or above was anemia (49%). Other grade 3 or higher TRAEs included infections (25%), cytokine release syndrome (24%) and neurological events (25%).2
Bijal Shah, MD, of the Lee Moffitt Cancer Center & Research Institute in Tampa, FL, discussed the results of the ZUMA-3 trial at the European Hematology Association Congress in 2021, saying, “For me, the three main takeaways are that we were able to treat patients safely and we were able to do so with a really high efficacy.”
Dr Shah also commented on the challenges of manufacturing CAR-T products, saying: “There’s always concern when it takes three or four weeks to turn around CAR T-cells.” However, Dr Shah highlighted promising CAR T-cell manufacturing results in the ZUMA-3 trial, saying, “In this particular trial, we were able to manufacture CAR T-cells with a median of about two weeks, and this is really incredible.”
The FDA approval of brexucabtagene autoleucel in October 2021 made it the first CAR-T therapy to be approved for the treatment of adult ALL. “I am really excited about this data. I think that [brexucabtagene autoleucel] is going to be a powerful adjunct for managing acute lymphoblastic leukemia,” said Dr Shah. “I’m really very eager to integrate it into the therapy for my patients, and I’m really hopeful that it will meaningfully change the benchmarks that we currently have.”
- US Food and Drug Administration. FDA approves brexucabtagene autoleucel for relapsed or refractory B-cell precursor acute lymphoblastic leukemia. US Food and Drug Administration (Online) [Last Accessed 19/10/2021].
- Shah BD, Ghobadi A, Oluwole OO, et al. KTE-X19 for relapsed or refractory adult B-cell acute lymphoblastic leukaemia: phase 2 results of the single-arm, open-label, multicentre ZUMA-3 study. The Lancet. August 2021. 7;398(10299):491-502.
Written by Elitsa Kamberska & Sophie Redfern
Edited by Thomas Southgate